Claudia Calder, a Ph.D. in Immunology and H&S consultant at Cardinus Risk Management, explains the science behind COVID-19, what we know of it, and provides some fascinating history into the vaccine.
COVID-19, or COronaVIrus Disease 2019, is a respiratory disease caused by a virus called SARS-CoV-2 (Severe Acute Respiratory Syndrome (SARS) Coronavirus 2).
Viruses have been around since life began forming. They have been described as organisms at the edge of life because technically viruses are not alive; they exist in a sort of intermediate netherworld, lying in wait until they can hijack a living cell and reproduce using the host cell’s metabolites.
There have been ten pandemics in the past 250 years, with 4 of them in the past 20 years.
A pandemic is defined as “An epidemic of an infectious disease that has spread across a large region, for instance, multiple continents or worldwide, affecting a substantial number of people.”
Three of the four pandemics in the past 20 years have been from the coronavirus family, SARS (or SARS-CoV-1) in 2002/3, MERS (Middle Eastern Respiratory Syndrome) in 2012, COVID-19 in 2019/20 and the fourth pandemic was the swine flu (influenza virus) in 2009. These viruses have led to diseases or conditions that affect the respiratory system and are easily spread throughout the human population.
Why have there been so many pandemics in the last 20 years?
As a species, humans are altering the way we interact with pathogens by venturing into rainforests and destroying them through logging, planting, and hunting for bushmeat; concentrating large numbers of people together in large cities; breeding millions of pigs and poultry (birds) and keeping them in close confines; and overusing and misusing antimicrobials (antibiotics). Humans are forcing pathogens (or germs) to adapt and giving them opportunities nature never did. We are helping spread these viruses because we are traveling more than ever.
The most dangerous place to live is where humans, pigs, and birds all live together in high numbers and close confines.
The SARS-CoV-2 did not come from either a pig or bird, it came from a bat via an intermediate animal, believed to be a Chinese pangolin, and ‘jumped’ into humans in the last week of November 2019, and then spread quickly around the world. By August 1, 2020, SARS-CoV-2 has been reported in 188 countries (of the world’s 195 recognized countries).
How and why does it spread so quickly?
There are a few reasons for this. One reason is that the common symptoms of COVID-19 (cough, fever, headaches, sore throat) are similar to flu and colds, so it is difficult to determine (certainly during the early stages of the pandemic) whether somebody just had a common cold or seasonal flu. It wasn’t until high numbers of people with shortness of breath resulting in breathing difficulties did medical professionals and those involved in the SARS pandemic in 2002/3 realized that COVID-19 was very similar.
The other reason for its rapid spread is that humans can transmit it from one person to another. Contact can occur from infectious respiratory droplets through coughing and sneezing. Another method is via surfaces (technically known as fomite). For example, where somebody has sneezed on a stainless-steel surface, the virus can survive up to 72 hours (but not reproduce) before being picked up by somebody else who touches their nose, mouth, and eyes and gets infected. More recent evidence has identified airborne transmission via breathing in tight spaces.
How does the virus get into the body?
To understand how SARS-CoV-2 enters the body, we need to understand what the virus expresses on its surface.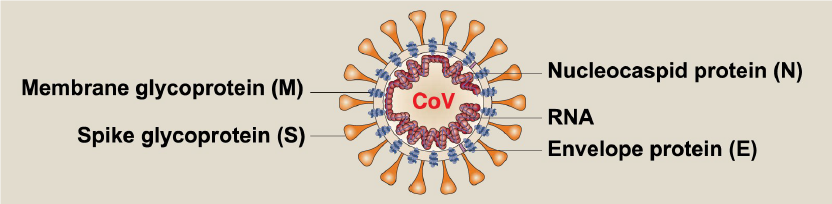
The virus (figure 1) is covered in a spike glycoprotein (also known as S protein). The S protein on the virus binds with a receptor called ACE2, which is expressed in humans on blood vessels, lung cells, the gut, and some parts of the brain. If you can imagine a human cell as a house, the ACE2 Receptor is the doorknob, the S protein binds to the Receptor, and the door opens so the virus can get into the cell. Once in the cell, the virus replicates, creating more viruses, eventually (though not in all cases) kills the cell releasing the virus into the body.
Once the virus is in the body, your response to the infection will depend on your genetics, health status, immune system, and several other factors (gender, age, etc.). There have been many symptoms associated with COVID-19 disease. The most common ones being high fever (your immune system trying to fight the virus), cough (irritation from the virus in your nose and throat), and shortness of breath (lung cells filling with fluid due to cell damage from when the virus has infected the cell). Other symptoms include anosmia (loss of smell) and dysgeusia (loss of taste). These symptoms occur as ACE2 Receptor is expressed on cells closely associated with neurons that interpret tastes and smells in the body.
How do the control measures stop the spread?
As discussed above, the COVID-19 virus spreads via respiratory droplets. To prevent ‘spreading the virus,’ you need to ‘catch’ your coughs and sneezes. This method will stop other people from breathing in the virus and prevent the virus from landing on surfaces, which can then be picked up by somebody else.
Physical distancing measures (i.e. standing 2m away from another person) reduces the likelihood of ‘catching’ the virus. Standing 2m apart minimizes the risk to 6% and 1m apart increases to 13% likelihood. The COVID-19 virus has a weak ‘membrane.’ Using soap and water can easily break it, which is why you should wash your hands regularly. If soap and water are not available, alcohol sanitizer will ‘fix’ the virus’s membrane, making the virus inactive.
The best way to protect yourself is to be as healthy as possible, avoid large crowds, regularly wash your hands, keep your distance from other people and be mindful of your own physical and mental wellbeing.
Vaccines – What are They and How Do They Work?
The term “vaccine” came about from the work of Edward Jenner in 1796. On May 14, he inoculated James Phipps, an 8-year-old boy. Jenner inoculated James with pus from cowpox blisters from a milkmaid, Sarah Nelmes. James developed a fever and some uneasiness but did not get the infection. Although James was challenged with other viral materials, no disease ever followed. James had been vaccinated successfully against smallpox.
Jenner, who referred to cowpox, the disease to which he exposed patients to immunize them from smallpox, as Variolae vaccinae, Latin for “smallpox of the cow.” The success of this means of inoculation against one of history’s greatest killers became known as “vaccination.”
Vaccines work by injecting individuals with a substance that resembles the disease-causing germ (such as SARS-CoV-2). The immune system recognizes the germs as a threat, and it mounts a response to destroy them – the immune system’s first-line defense (called innate immunity). One of the clever things that the immune system does when challenged with a vaccine is to produce molecules, such as antibodies, which is known as a secondary defense system (or adaptive immunity). This part of the immune system can recognize any subsequent germ from the vaccination and can mount a response and destroy the germs, resulting in no disease in the vaccinated person.
There are multiple ways to make vaccines, depending on the germ/disease in question. Regarding vaccines against SARS-CoV-2, the most famous vaccine is from Pfizer/BioNTect, first used in the UK on December 9, 2020.
Historically, vaccines are made by making the germ “dead” or “inactive” and injecting this into an individual, and this stimulates the immune system (as described above). The Pfizer/BioNTect vaccine is an mRNA vaccine. It works slightly differently, but the outcome is the same. The vaccine teaches the adaptive immune system how to identify the virus and then destroy it.
Having a Vaccine is Great, but We Must be Vigilant in Keeping the Virus and Disease at Bay
Having a vaccine against COVID-19 is the best news to come out of 2020. However, as Walter Orenstein (former CDC director of the USA Immunisation Programme and former Bill & Melinda Gates Foundation Deputy Director for Immunisation Programmes) put it in 2019 after a career spanning almost 50 years:
Vaccines don’t save lives. Vaccination programs save lives (Orenstein, 2019).
It won’t be until at least 70% of the population has been vaccinated will the control measures – social distancing, washing hands, and covering your nose/mouth – be reduced.
We must continue to be stringent in carrying out these control measures to protect those we love (especially the older population).
The best way to protect yourself (and others) is to be as healthy as you can be by avoiding large crowds, regularly washing your hands, keeping your distance from other people, and being mindful of your own physical and mental wellbeing.
Biography:
Claudia Calder is a health and safety consultant at Cardinus and brings with her a unique set of skills, specializing in medical, biological, and laboratory safety. A Ph.D., she has a rich academic background which she applies to safety, health, and environmental consultancy.