COVID-Safe Handbook
Your guide to managing the safety risks presented by COVID-19.
COVID-Safe Handbook
The COVID-19 pandemic has had an impact on everybody's life around the world.
This handbook, which is also available as a PDF, provides a simple guide to what COVID-19 is, how it is caused, and the control measures you can implement to keep you and others safe. I’ve put this together over the course of the pandemic, and while new information appears frequently, the information presented here should stay relatively stable. Much of this information can be found on our COVID-19 H&S Hub.
Dr Claudia Calder, H&S Consultant, [email protected]
COVID-19 – What Is It?
COVID-19, or COronaVIrus Disease 2019, is a respiratory disease caused by a virus called SARS-CoV-2 (Severe Acute Respiratory Syndrome (SARS) Coronavirus 2).
Viruses have been around since life began forming. They have been described as organisms at the edge of life because technically they are not alive, they exist in a sort of intermediate netherworld, lying in wait until they can hijack a living cell and reproduce using the host cell's metabolites.
In the past 250 years, there have been 10 pandemics, with 4 of them in the past 20 years.
A pandemic is defined as 'An epidemic of an infectious disease that has spread across a large region, for instance multiple continents or worldwide, affecting a substantial number of people'.
Coincidentally 3 of the 4 pandemics in the past 20 years have been from the coronavirus family, SARS (or SARS-CoV-1) in 2002/3, MERS (Middle Eastern Respiratory Syndrome) in 2012 and COVID-19 in 2019/20 and the fourth pandemic was the swine flu (influenza virus) in 2009 – all these viruses have lead to diseases or conditions that affect the respiratory system and are really easily spread throughout the human population.
Why Have There Been so Many Pandemics in the Last 20 Years?
Humans are altering the way we interact with pathogens, by venturing into rain forests and destroying them through logging, planting and hunting for bushmeat; concentrating large numbers of people together; breeding millions of pigs and poultry (birds) and keeping them in close confines; by overusing and misusing antimicrobials drugs (antibiotics); humans are forcing pathogens (or germs) to adapt to continual stresses and giving them opportunities nature never did. And we are helping spread these viruses, because we are travelling more globally more than we ever have in history.
In fact, from a pandemic perspective, the most dangerous place to live is where humans, pigs and birds all live together in high numbers and close confines.
However, SARS-CoV-2 did not come from either a pig or bird, it came from a bat via an intermediate animal, believed to be a Chinese pangolin, and 'jumped' into humans in the last week of November 2019, and then spread quickly around the world, by the 1st August 2020 SARS-CoV-2 has been reported in 185 countries (there are 195 recognised countries in the world) (Rothan, H.A. and Byrareddy, S.N., 2020. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of autoimmunity, p.102433; Shereen, M.A., et al., 2020. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research).
How and Why Does it Spread so Quickly?
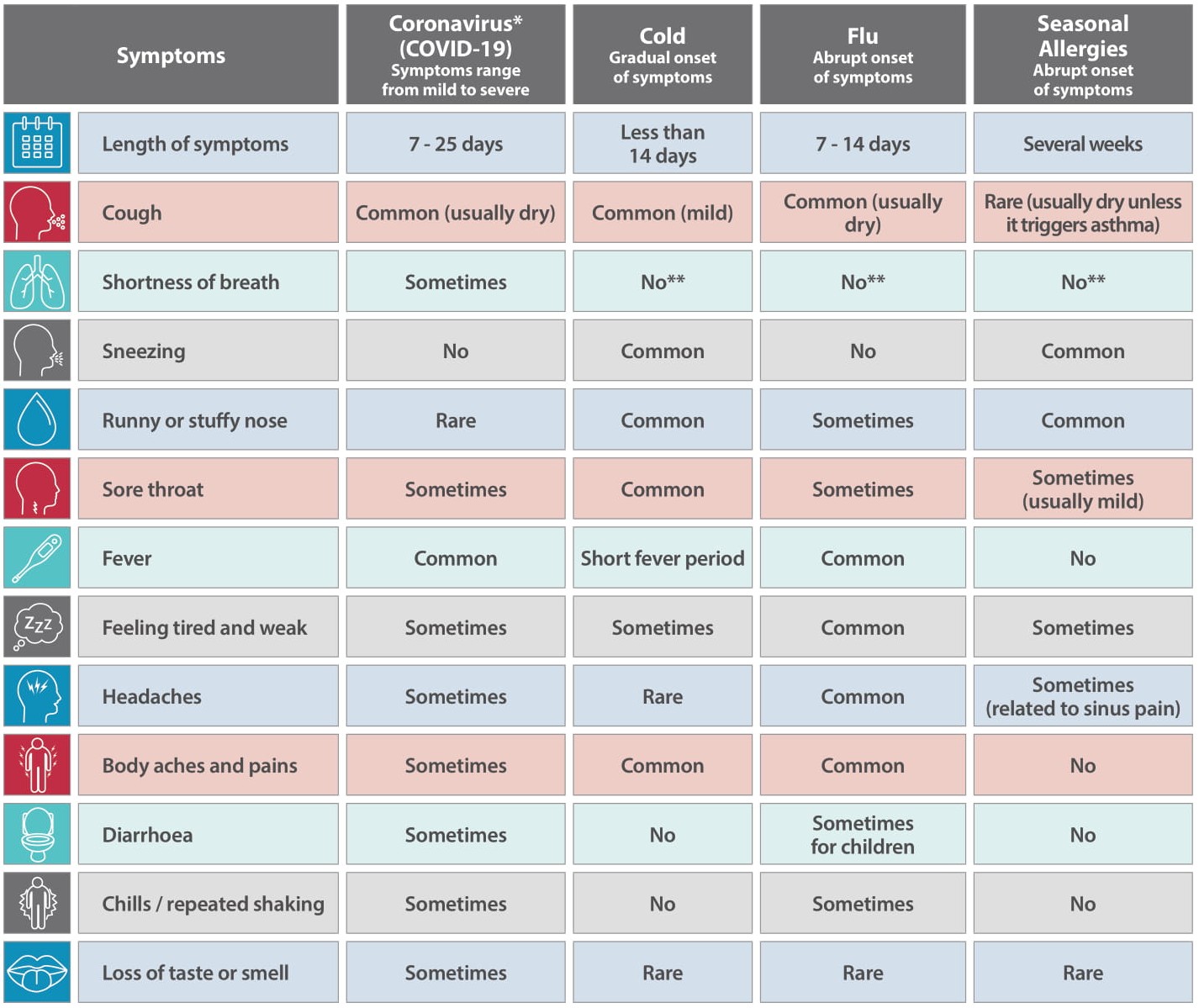
There are a few reasons for this, one reason are the common symptoms of COVID-19 (cough, fever, headaches, sore throat) are similar to flu and colds, so it is difficult to determine (certainly during the early stages of the pandemic) whether somebody just had a common cold or seasonal flu, and typically most people who had these symptoms assumed that they had a cold and just got on with their daily lives.
It wasn't until high numbers of people started having shortness of breath which resulted in difficulties in breathing, where people were being admitted into hospitals, did medical professionals realise something else was going on, and those involved in the SARS pandemic in 2002/3 realised that COVID-19 was very similar.
Other reasons how and why it spreads so quickly is because of how humans can transmit it from one person to another. We have all heard of the R number, this is the reproduction number, in March 2020 the R number in the UK was 3, meaning that it one person had it, on average they would spread it to 3 other people.
Contact from infectious respiratory droplets through coughing and sneezing is one method of transmission, the spread via surfaces (technically known as fomite), where if somebody for example sneezed on a stainless steal surface, the virus can survive up to 72 hours (but not reproduce) before being picked up by somebody else who touches their nose, mouth and eyes and gets infected. And more recent evidence of airborne transmission via breathing in close spaces. (Domingo, J.L., et al., 2020. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environmental Research, p.109861).
How Does the Virus Get Into the Body?
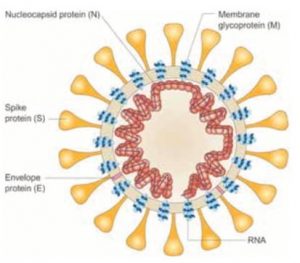
To understand how SARS-CoV-2 enters the body, we need to understand what the virus expresses on its surface.
The virus (figure 1) is covered in a spike glycoprotein (also known as S protein). The S protein on the virus binds with a receptor called ACE2 which is expressed in humans on blood vessels, lung cells, the gut and some parts of the brain.
Simply put, if you can imagine a human cell as a house, the ACE2 Receptor is the doorknob, the S protein binds to the receptor and the door is opened and the virus can get into the cell. Once in the cell, the virus replicates, creating more virus, eventually (though not in all cases) kills the cell releasing the virus into the body (Zhang, H., et al., 2020. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive care medicine, 46(4), pp.586-590).
Once the virus is in the body, depending on your genetics, health status, immune system and a number of other factors (gender, age, etc) will depend on how your body responses to the infection. There have been a number of symptoms associated with the COVID-19 disease with the most common ones being high fever (this is your immune system trying to fight the virus), cough (irritation from the virus in your nose and throat) and shortness of breath (lung cells filling with fluid due to cell damage from when the virus has infected the cell).
Other symptoms include anosmia (loss of smell) and dysgeusia (loss of taste), these symptoms occur as ACE2 receptor is expressed on cells closely associated with neurons that interpret tastes and smells in the body (Brann, D.H., et al., 2020. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Science Advances, p.eabc5801).
What Do You Do if You Develop Symptoms?
First thing is to self-isolate and ask those in your household or bubble to do the same. Government guidance has changed recently and now states that you need to self-isolate for 10 days from the start of your symptoms and your household (or bubble) to self-isolate for 14 days from the start of your symptoms.
If you are working, you should let you line manager or supervisor know, this is particularly important if you are working on-site, rather than working from home, as your workplace can then implement their track and trace procedure. Next thing is to arrange to be tested – you should get tested within 3 days of your symptoms starting – you can do this by contacting the NHS on 111 or via the online coronavirus service (https://111.nhs.uk/covid-19), you will need to stay at home until you receive your test results.
If you test negative, great! You and your household are free to stop self-isolating. If you test positive, the NHS will provide guidance on what to do if your symptoms get worse.
There are currently two available tests, the main test – called a PCR test – looks at whether you have virus in your body, by looking for the virus' genetic material, the best time to have this test is within 3 days of your symptoms showing.
This is the test where medical professionals use a swab on your nose and throat. The other test – called an Antibody test – looks at whether your immune system has made antibodies to the virus, which basically means, if your body has 'seen' the virus by taking your blood.
The best time to have the antibody test is 3 weeks after the start of your symptoms, when the antibodies are at their highest level. The antibody test does not tell you whether you are protected against being re-infected with the virus. As the virus has only been known for 9 months, it is difficult to know whether the immune system's production of antibodies will protect in the future.
This is how the vaccine works, by making your immune system produce antibodies, which 'neutralise' the virus, removing it from your system, so you do not develop the disease.
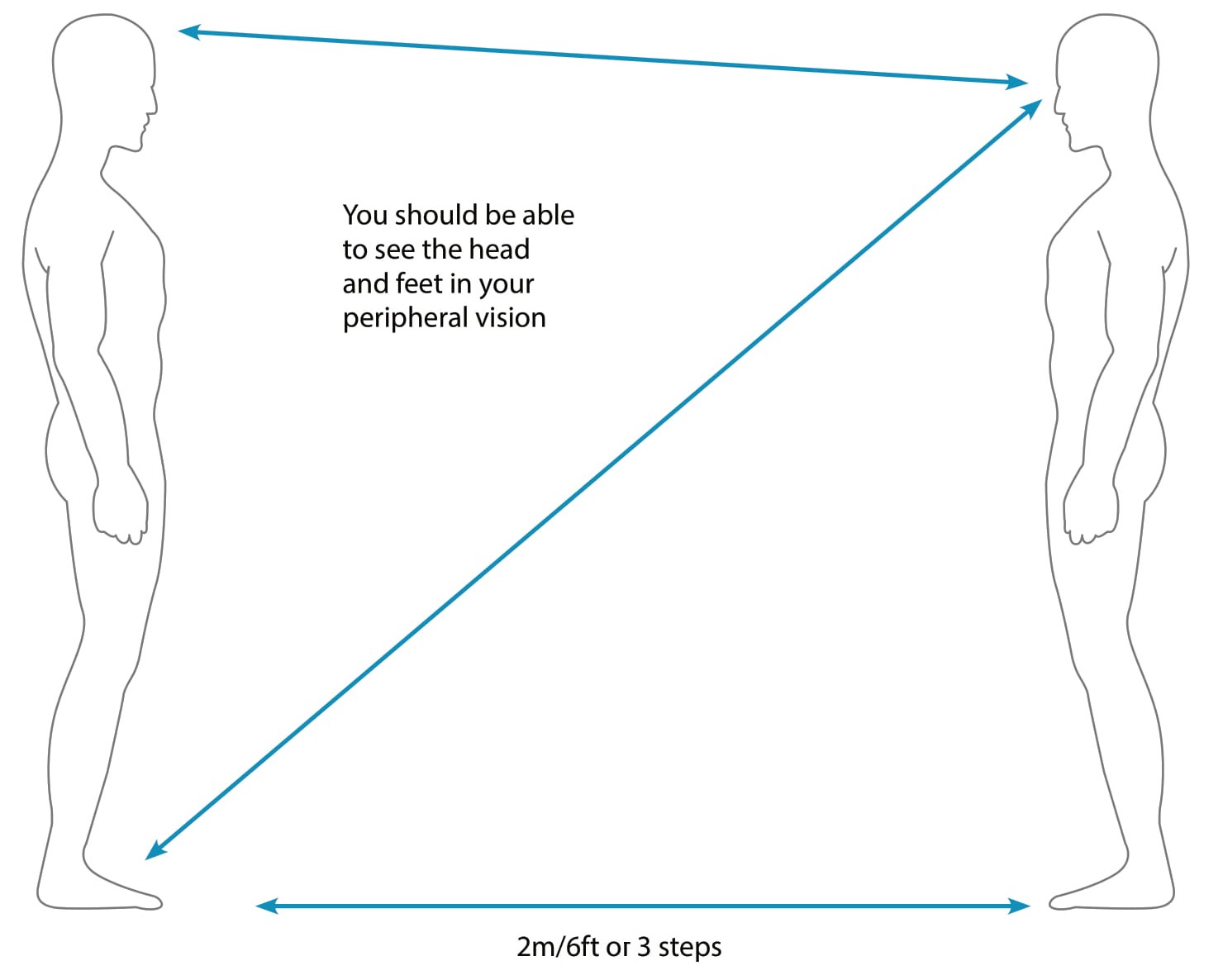
Physical Distancing
Physical Distancing
Currently physical distancing measures stand at 2m. If you cannot be 2m apart, try to keep at least 1m whilst wearing a mask (or other type of mitigation). The best measure is to try and keep 2m apart (or more), the easiest way of working this out is ensuring that you can see the head and feet of the person that you are dealing with (as long as they are standing up). Another way is being at two arm's length, one arm length of you and the second arm length of the person you are interacting with.
PPE and RPE
Personal Protective Equipment and Respiratory Protective Equipment
PPE stands for Personal Protective Equipment and covers items such as gloves, to protect hands and face shields (or visors) to protect the face and eyes. RPE stands for Respiratory Protective Equipment, namely face masks and respirators, which protect your respiratory system (nose, throat and lungs).
PPE and RPE has been designed to protect an individual user, based on the individual's needs (e.g. shape of face, any allergies, etc), the task and the environment in which they will be working. PPE and RPE is known as the last resort in the hierarchy of controls as they are least effective of the controls.
PPE and RPE should never be shared once worn/used, think of it like a toothbrush, you would never share that with anyone, never share your mask or face shield with anyone, even close family members.
Gloves
The use of gloves will protect your hands from all sorts of things, including viruses and chemicals. However, it is important to remember that you can still transfer 'stuff' from your gloves as you would your hands, for example, if you touch your face whilst wearing your gloves.
Wear gloves made of nitrile, these have been shown to be most effective in protecting against viruses and are the least likely material to have an allergic reaction to.
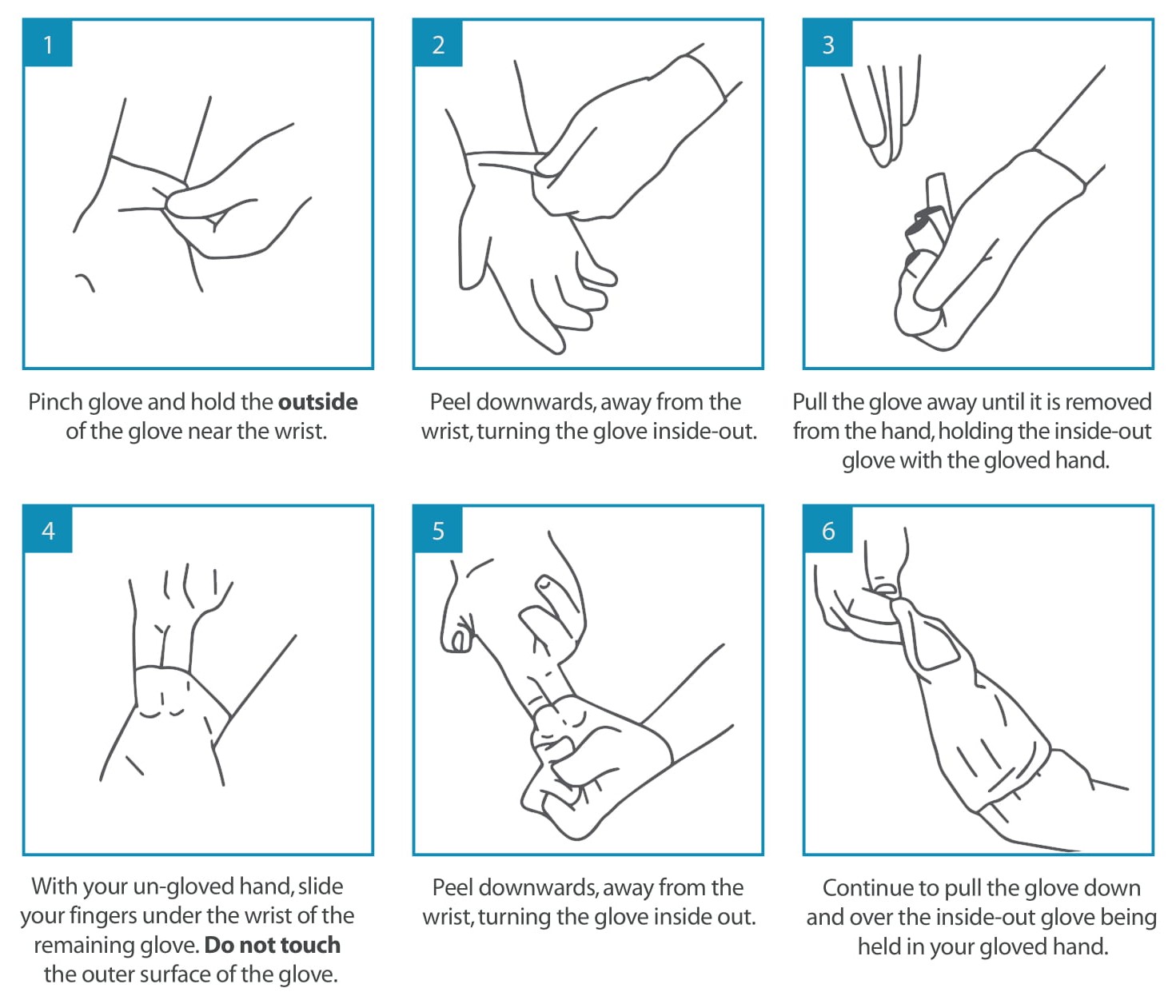
It is really important to ensure that you take your gloves off properly, by doing this ensures that there is no contamination and the gloves, once disposed are inside out, meaning that if there is virus on them, the virus is 'trapped' in the glove and can't be re-aerosolised.
Wearing gloves – wash hands before putting gloves on, make sure that your hands are dry, it is not easy putting on a glove with damp hands. Once you take your gloves off, wash and dry your hands. Do not re-use disposable nitrile gloves.
Make sure you take of your hands. You know your hands the best, if you start seeing any reddening or flaky skin once you start wearing gloves regularly, use a barrier cream or moisturiser. In extreme cases, the use of gloves can lead to dermatitis (inflammation of the skin), if this happens, see your general practitioner who will be able to advise.
Glove Removal
Face shield (or Visor)
A face shield is designed to prevent 'splash-back' of liquids (or respiratory droplets) from getting on your face and into your eyes, they do not protect your respiratory system, meaning that you can still 'breathe' in the virus.
Face shields can be annoying as they can steam up, a little trick to help to prevent this is to put a little bit of washing up liquid on the inside, not much so you can still see out it.
Face shields are re-usable, like all PPE should never be shared. Once you receive your face shield, put your initials (or name on it) and keep the bag. At the end of your shift, clean the face shield (inside and out) with an alcohol wipe or use soap and water, put it in the bag and place in your locker. You should only need to replace your face shield if the visibility becomes a problem (this is normally through scratches on the surface) or if the elastic band breaks.
Face Mask
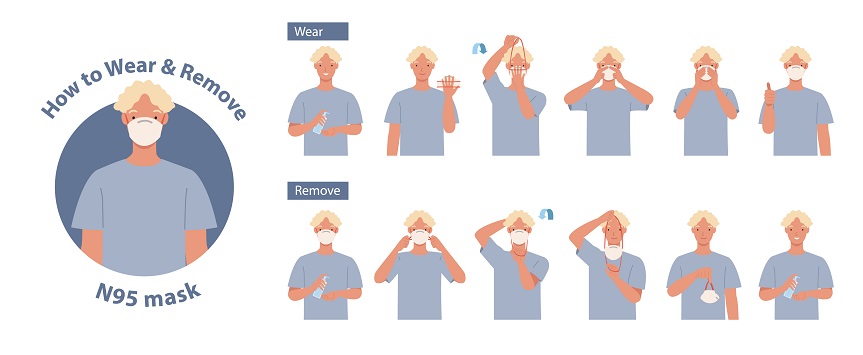
A face mask is designed to protect your respiratory system. Unless it has been face-fitted by a competent RPE face fitter, it is not 100% effective. Just because you are wearing a face mask, does not mean that you are completely protected, especially if you have a beard.
When wearing a face mask, make sure of the following for best protection:
- Wash your hands before putting on your face mask and wash your hands once you have removed the face mask
- Try not to touch the 'inside' of the mask (the part that touches your mouth)
- You have a good seal around the top of the nose and chin
- For the top of the nose, squeeze the plastic strip down on your nose and cheekbones (if you are a glasses wearer, this will help with reducing your glasses from steaming up)
- Avoid pulling the mask down and letting it hang on your chin or round your ears, the best thing is to just take it off and put it in your pocket. If you wrap it around your wrist (for example) you risk the chance of transferring the virus (or anything else, you have on your skin) into your respiratory tract
How to Wear and Remove a Face Mask
Hierarchy of Controls
Safety experts use a system called 'Hierarchy of Controls' to eliminate or minimise exposure to hazards, which ranks the effectiveness and efficiency of hazard controls.
Simply put, it is a system where you start at the top of the hierarchy and try and put in appropriate control measures at each stage, until you have eliminated, or minimised as much as possible, the risk.
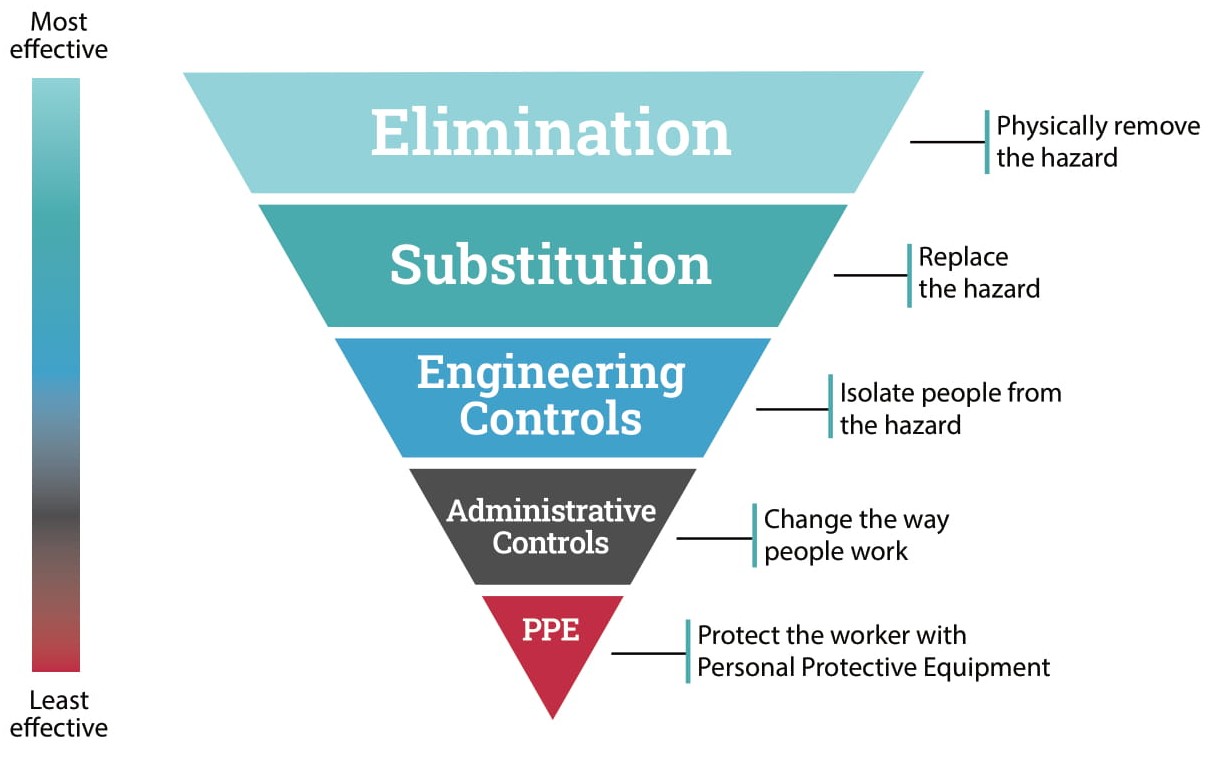 Elimination – Physically Remove the Hazard
Elimination – Physically Remove the Hazard
To eliminate COVID-19 in the population, the virus needs to 'go away'. To do this, a vaccine needs to be developed and administered to the population, so that we are protected from developing the disease from the virus. There is no way of 'killing' the virus all at once unless somebody develops an airborne neutralising anti-viral vector, which is currently impossible to do. Sadly, we don't live in the movies!
Substitution – Replace the Hazard
We cannot substitute COVID-19 for something else, however, when cleaning our hands, we can substitute alcohol-based sanitiser, which can cause dermatitis, for soap and water.
Engineering Controls – Isolate people from the hazards
This is the stage where we can start minimising the risk against COVID-19 in the workplace. COVID-19 is transmitted person-to-person through respiratory droplets from coughs and sneezes, and possibly breath.
This is why advice from the UK Government is to catch your coughs and sneezes in a tissue (or the crease of your elbow) and to keep 2m apart from each other – isolating people from the hazard, which are other people.
Physical engineering controls such as plastic screens have been put in place in shops to protect customer service staff from customers, as well as physical distancing measures. Office environments have also put screens in between workstations to minimise the risk of transmission between workers.
At this stage, we have slightly reduced the risk to the transmission, under certain working environments. So, what can we do next to reduce the risk even further?
Administrative Controls – Change the Way People Work
Administrative controls include training, procedure, policy or shift designs that reduce the risk of a hazard to an individual, typically changing the behaviour of people, rather than actually removing the hazard.
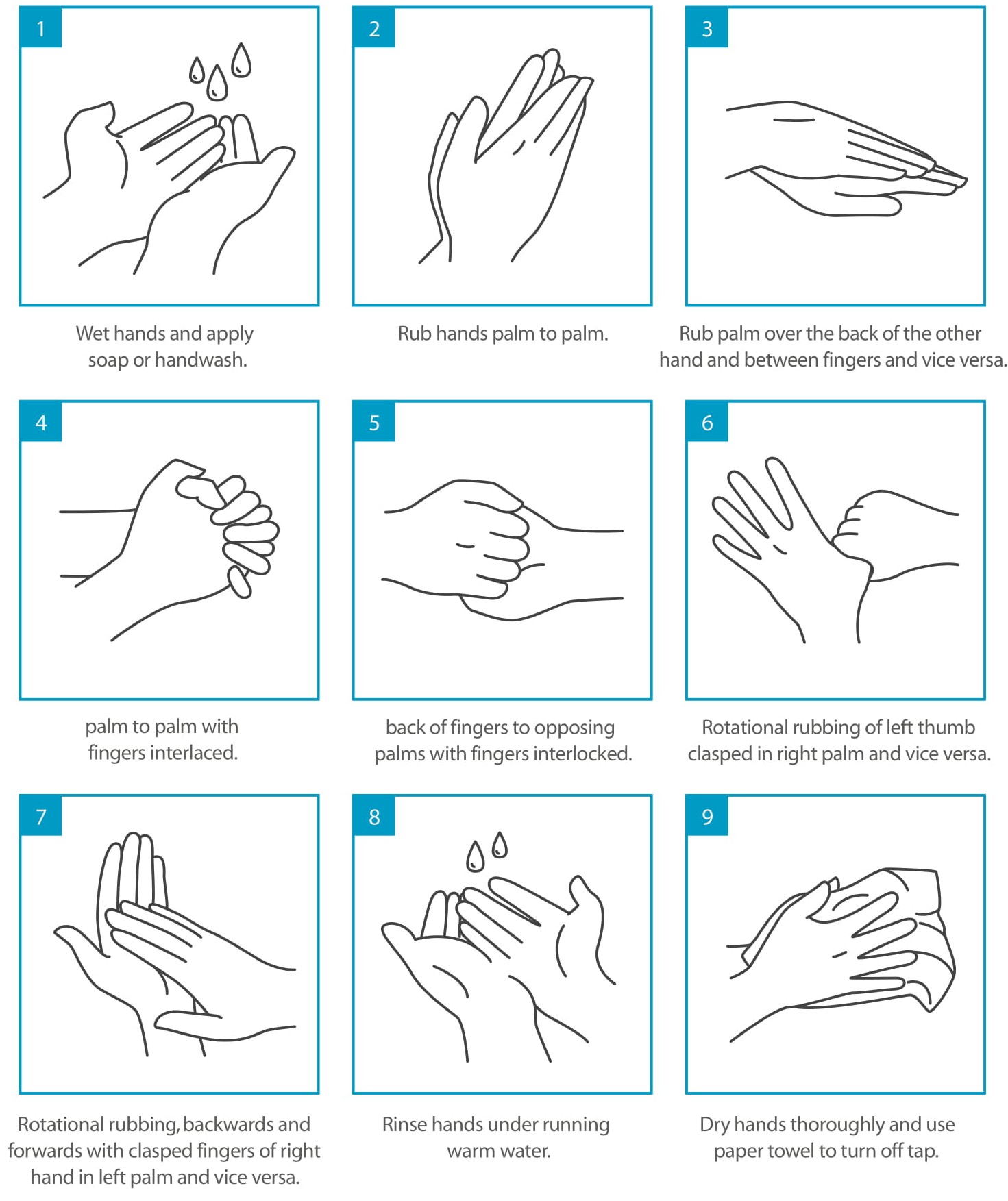
As we start to return to work, whether it be in an office or factory or shop, workers are going need to change their behaviour to include washing hands (good hygiene practices) and physical distancing.
This already started to become 'normal', but these messages will need to be reinforced in the workplace, as we will forget to do these things. We need to recognise that our environment sometimes directs our actions – for example, last time we were in the office, we chatted in the kitchen, just got into the lift with whoever, in the COVID-19 world, we just won't be able to do this without thinking of the potential consequences.
Your return to work/COVID-19 risk assessment will lay out what control measures will need to be brought in – if you are struggling with this, please contact our safety consultancy team, we can help you through this process and provide you with an induction program, as well as bespoke documentation for your organisation.
Some considerations to think about include:
- Training your workforce in good hygiene practices, reinforcing these messages with posters, emails and screensavers
- Strengthening the message, that if you have any COVID-19 symptoms (prolonged cough and fever) or have been near people who have these symptoms to stay at home
- Communicating and reinforce your procedures and policies to your workforce through e-learning or alternative communication mediums
- Leading by example
At the end of stage 4, we have now minimised the risk to exposure somewhat, but what about those workers who come into contact with lots of people, such as public transport or frontline work, where the viral load (how much virus is around) is higher than you would expect in a workplace?
Personal Protective Equipment (PPE) – Protect the (Individual) Employee
PPE is the final stage of the hierarchy of controls and is to be used when engineering or administrative controls are not feasible or effective to reduce the risks to acceptable levels.
First Aid in the COVID World
First Aid in the COVID World
First aid for minor incidents can be delivered by anyone, however, if in doubt call your trained first aiders and/or the emergency services.
Providing First Aid
Where possible, try and get the casualty to administrate self-aid with your support.
Be aware of the risks to yourself and others
In the event that somebody needs emergency first aid at work, go through the normal triage process and call the emergency services if necessary.
Keep yourself safe
- Wash your hands before and after treating a casualty
- Ensure you do not sneeze or cough over the casualty when you are treating
- Wear gloves or cover hands when dealing with open wounds
- Cover cuts and grazes on your hands with waterproof dressing
- Dispose of all waste safely – in hazardous waste, if available or double bag and put in 'normal/black bag' waste or use sanitary bins (found in ladies' toilets)
Give early treatment
The vast majority of incidents do not involve you getting close to the casualty, where you could come into contact with respiratory secretions. Sensible precautions will ensure you are able to treat a casualty effectively.
Information
Information about COVID-19 is being continually updated by the government and the NHS, keep yourself informed and updated.
Remember your own needs
Make sure you take time to talk about your fears and concerns with someone you trust and to take out time to look after yourself.
Heart Attack
Heart Attacks can come in two forms:
- Myocardial infarction (MI), this is when blood vessels leading to the heart become blocked, the heart can still pump blood around the body and the person will be conscious and breathing. MI can lead to cardiac arrest.
- Cardiac Arrest is when the electrical activity of the heart becomes abnormal leading to the heart to stop pumping blood.
Symptoms – men and women do not experience heart attacks in the same way:
- Both genders
- Chest pressure/pain/discomfort
- Feeling dizzy
- Rapid or irregular heartbeat
- Shortness of breath
- Back, neck, arm or jaw pain
- Women
- Unusual fatigue
- Anxiety and sleep disturbances
- Nausea
- Men
- Pain in left arm
- Breaking out in cold sweat
- Stomach discomfort or indigestion
CPR (Cardio-Pulmonary-Resuscitation)
Because of the heightened awareness of the possibility that the patient may have COVID-19, Resuscitation Council UK offers this advice:
- Recognise cardiac arrest by looking for the absence of signs of life and the absence of normal breathing. Do not listen or feel for breathing by placing your ear and cheek close to the patient's mouth. If you are in any doubt about confirming cardiac arrest, the default position is to start chest compressions until help arrives
- Make sure an ambulance is on its way. If COVID-19 is suspected, tell them when you call 999
- If there is a perceived risk of infection, rescuers should place a cloth/towel over the patient's mouth and nose and attempt compression only CPR and early defibrillation until the ambulance (or advanced care team) arrives. Put hands together in the middle of the chest and push hard and fast, 1/3 of their chest size and a rate of 100 per minute
- Early use of a defibrillator significantly increases the person's chances of survival and does not increase risk of infection
- If the rescuer has access to personal protective equipment (PPE) (e.g. FFP2 face mask, disposable gloves, eye protection), these should be worn.
- After performing compression-only CPR, all rescuers should wash their hands thoroughly with soap and water; alcohol-based hand gel is a convenient alternative.
They should also seek advice from the NHS 111 coronavirus advice service or medical adviser.
The below video is an excellent visual aid.
Stroke
A stroke is a very serious condition where the blood supply to part of the brain is cut off. A stroke can be caused by either a blood clot in the brain or bleeding in the brain. It needs to be treated in hospital as soon as possible.
Common symptoms of a stroke include the face dropping on one side, not being able to lift the arms and slurred speech.
Using the pneumonic FAST, you will be able to tell whether somebody has had a stroke:
F – Face – has the face dropped on one side? Ask the person to smile. This might be difficult to know if somebody is wearing a face mask.
A – Arms – can the person lift their arms? Ask the person to raise both of their arms.
S – Speech – can the person talk properly? Ask the person to repeat a phrase ('Danger is no Stranger to a Rainbow Ranger!!' – or something simple such as 'Mary had a little lamb')
T – Time – phone for an ambulance (999/112) – also note the time that the stroke or incident occurred, this will help with treatment at the hospital.
Sprains
Slips, trips and falls at same height normally result in sprains, in some cases and depending on where this has occurred may result in broken bones or other injuries. For simple sprains, use the pneumonic RICE to treat the injured party.
R – Rest – rest the injured part of the body
I – Ice – ice the injured part of the body, you could use a bag of frozen peas, or an instant cold pack (which can be found in some first aid kits), or ice wrapped in a towel (or other material)
C – Compress – using a bandage (or other material) wrap compress around the injured part
E – Elevate – elevate the injured part. For ankle sprains, raise the ankle using a pillow or something similar.
Keeping Yourself Healthy
Keeping Yourself Healthy
There are three key areas on keeping yourself healthy – sleep, diet and exercise. All are linked together, for example, getting a good night's sleep will help with your exercise or training the next day, having a good healthy meal consisting of vegetables provides you will the fuel to carry out your exercise or training and will also help with sleeping.
Top Tips for Sleeping
Handy hints on why you should sleep and how you get a good night's sleep.
Sleeping 7-9 hours at night is probably the single most healthy thing you can do for yourself.
Why?
Routinely sleeping less than six or seven hours at night has devasting effects on your body:
- Affects your immune system, more than doubling your risk of cancer
- As a lifestyle factor to determine whether or not you develop Alzheimer's disease
- Disrupts blood sugar levels to the point where you may be classified as pre-diabetic
- Increases likelihood of coronary arteries becoming blocked and brittle, leading to cardiovascular disease, stroke and congestive heart failure
- Contributes to all major psychiatric conditions, including depression, anxiety and suicidality
- Increases the concentrations of a hormone that makes you feel hungry while suppressing a companion hormone that otherwise signals food satisfaction – despite being full, it makes you want to eat more, leading to weight gain
Added all up – the shorter you sleep, the shorter your life span
So, what can you do to get a good night's sleep? Here are 12 top tips:
-
Have a sleep schedule – Go to bed and wake up at the same time each day. Sleeping later on weekends doesn't fully make up for a lack of sleep during the week and it will make it harder to wake up on Monday morning.
- Set an alarm – For both waking up and going to bed
-
Exercise – Doing exercise or any physically activity is great, doing a minimum of 30 minutes a day is great for your health, but try not to exercise for 2-3 hours before going to bed, as your body temperature will be higher which makes falling asleep a little difficult – your brain likes to sleep in slightly cooler climates
- Sleeping helps with exercise – If you get a good night's sleep, this will help with your exercise the following day, giving your more energy to workout
- Avoid caffeine and nicotine – Coffee, tea (some types), colas, chocolate all contain caffeine, which is a stimulant, and its effects can take up to 8 hours to wear off fully. Therefore, having a cup of coffee in the late afternoon, may perk you up, but it will have a knock-on effect to your night's sleep. Nicotine is also a stimulant, often causes smokers to have a lighter sleep, smokers also wake up early due to nicotine withdrawal.
- Avoid alcoholic drinks before bed – Having a nightcap (or alcoholic beverage) before bed may help you to relax, but heavy use deprives you of REM sleep, keeping you in the lighter stages of sleep. Heavy alcohol usage also may contribute to impairment in breathing at night. When the effects wear off in the middle of the night, it tends to wake you up.
- Avoid large meals and beverages at night – A light snack is okay – you don't want to go to bed too full or too hungry – a large meal can cause indigestion, which interferes with sleep. Drinking too many fluids will cause you to wake up to urinate.
- Wherever possible, avoid taking medications that delay or disrupt your sleep – Commonly prescribed heart, blood pressure, or asthma medications, as well as some over the counter and herbal remedies for coughs, colds or allergies, can disrupt sleep patterns. If you are having trouble sleeping, talk to your healthcare provider to see if the drugs you are taking are contributing to your insomnia and ask if you can take them at different times of the day, to help you sleep.
- Don't take naps after 3pm – Naps can help make up for lost sleep, however, napping too late in the day can make it harder to fall asleep at night.
- Relax before bed – Schedule time at the end of the day for unwinding. A relaxing activity, such as reading or listening to music, should be part of your bedtime routine. If you are going to read, just be aware, if you are using an electronic device to read, the LED light can 'wake' up your brain, making it a little more difficult to fall asleep.
- Take a hot bath before bed – The drop in body temperature after getting out of the bath, might make you feel sleepy, and the bath can help you relax and slow down, so you are more ready to sleep.
- Dark bedroom, cool bedroom, gadget-free bedroom – Remove anything in your bedroom that might distract you from sleep, such as noises, light, an uncomfortable bed and warm temperatures. If the temperature of your bedroom is on the cool side, this will help you sleep better. TV, phones and other gadgets in the bedroom can be distractions and deprive you of sleep, set a deadline when you are going to last check your email/Facebook/Twitter, try and set this to at least 1 hour before you go to bed, and then leave your device outside the bedroom, so you are not tempted to check it. Having a comfortable mattress and pillow can help promote a good night's sleep – if you are having trouble sleeping, then now might be the time to invest in a new mattress and coverings. If you find yourself clock-watching in the night, turn the clock around so you cannot see it, and don't worry about what time you fall asleep.
- Have the right sunlight exposure – Daylight is the key to regulating daily sleep patterns. Try and get outside in natural sunlight for at least 30 mins a day. If possible, wake up with the sun or use bright lights in the morning. Sleep experts recommend you should get an hour of sunlight exposure in the morning and turn the lights down before bedtime.
- Don't lie in bed awake – If you find yourself still awake whilst in bed for more than 20 minutes or you are starting to feel anxious or worried, get up and do some relaxing activity until you feel sleepy (try not to put bright lights on). The anxiety of not being able to sleep can make it harder to fall asleep.
Information adapted from Why We Sleep by Professor Matthew Walker. Penguin Books, 2017.
Top Tips to Improve Wellness through Movement
Exercise or movement is a miracle cure that has always been available, but for too long people have neglected to carry out the recommended amount, and the consequence of this is our health is now suffering.
Scientific evidence shows that being physically active can help you lead a healthier and happier life.
People who regularly exercise have a lower risk of developing many long-term or chronic illnesses, such as heart disease (up to 35% lower risk), type 2 diabetes (up to 50% lower risk), stroke (up to 35% lower risk) and some cancers (e.g. up to 20% lower risk for breast cancer). Furthermore, physical activity can also boost self-esteem, mood, sleep quality and energy, as well as reducing your risk of stress, depression and dementia (up to 30% lower risk).
To stay healthy, adults should try and be active every day and aim to achieve at least 150 minutes of physical activity over a week through a variety of activities.
For most people, the easiest way to get moving is to make activity part of your everyday life, like walking or cycling. However, the more you do, the better. And taking part in activities such as sport and exercise will make you even healthier.
For any activity to benefit your health, you need to be moving quick enough to raise your heart rate, breathe faster and feel warmer, this level of effort is called moderate-intensity activity, where you should be able to talk but not sing words to a song.
Vigorous activity, where you work harder than moderate activity, has been shown to bring bigger health benefits. You can tell if you are working harder because your breathing harder and faster, and your heart rate has gone up quite a bit, you should only be able to say a few words without pausing for breath.
To start getting into exercise, the easiest thing to do is to start walking.
Top Tips to Start Walking
 All you need are your legs, you don't need specialised equipment or a gym membership. Walking can help you lose body fat and improve your joint health, circulation, bone density, sleep cycle, blood pressure and mood.
All you need are your legs, you don't need specialised equipment or a gym membership. Walking can help you lose body fat and improve your joint health, circulation, bone density, sleep cycle, blood pressure and mood.
Set Goals – When you start set a realistic goal, if 20 minutes a day leaves you exhausted and sore, then try 10 minutes on alternative days, and then raise it up by 2-5 minutes each week as you build your fitness. Once you hit your goal, start adding more days or increase the duration. Once you are more comfortable, try a more challenging workout, increase your speed or find a route with hills.
Set a Schedule – If you are an early riser and like to get things done in the morning, then do your walk first thing. If evenings are better, do it then. Write the time in your calendar and try and stick to it. Better yet, make a regular appointment with a friend, so it is harder to skip.
Get Going – To improve try to set a schedule of 150 minutes during the week, which works out as 30 mins a day, however, doing 5 minutes a day is better than doing nothing. The more you do, the better your health.
Get the Right Shoes – You want a shoe that has decent padding, with a material that 'breathes', that is water-resistant and has flexibility from heel to toe. The most important thing is the fit of the shoe. Your shoes should be loose enough so that you can wiggle your toes with ease, but snug enough so your foot doesn't slide around.
Clothes – Any type of clothing will work. If it is cold, wearing layers is better as you can remove them as you get warmer. If it is sunny, think about how you can protect yourself from the sun, wearing a hat, sunglasses and sunscreen will protect you. Your phone might be a useful way to track your distance, most phones have a built-in health app that can either track distance and/or the number of steps – don't forget to charge your phone, just in case of emergencies or you need it for a map.
Integrating Walking as Part of Your Day – think about the places that you go during the day and ask yourself 'could I walk there?'. Think about parking the far end of the car park (as long as it is safe to do so), take the stairs instead of the lift, if you use public transport, could you get off at an earlier stop and walk the rest of the way?
Alternate Plans – There are many reasons to skip a walk, like bad weather, or a long workday, or low energy. If you make exercise a priority, you are more likely to fit it in your day. Look at alternatives, if you normally walk first thing in the morning, but got up late, could you take a walk on your lunch break? If it is too rainy or too cold, are there any alternative places you could walk, such as an indoor shopping centre? If you need to miss a day, plan to make up the time, for example, if you are aiming to 30mins a day, but miss a day, just add an additional 5 mins onto the other days – every little helps.
Keep Track – There are lots of gadgets and apps available that can tell you how far you have gone, some even have how many calories you have burned, this is a good way of setting goals and seeing your improvement.
Drink Water – The more you exercise the more you sweat. When you become dehydrated (your water levels are too low) you might feel tired, sick, dizzy or confused. Top up your tank by drinking a couple of extra glasses of water in the hours before you head out for your walk or take a water bottle with you when you go for your walk, this is especially important if it is really hot outside or you are going a long way.
Top Tips for Eating to Improve Wellbeing
 Handy hints on why you should eat well and how you can start incorporating healthier options into your diet.
Handy hints on why you should eat well and how you can start incorporating healthier options into your diet.
The old wives' tale of 'you are what you eat' is true.
Eating a healthy, balanced diet is an important part of maintaining (and improving) good health, helping you feel better, both mentally and physically.
The key to eating for wellness is not necessarily what foods to eat, but rather how and when we eat them.
Why Does Food Influence How We Sleep, Feel and Interact with People?
Food influences the way we feel, how we sleep and interact with other people. Too much food can lead to extra weight, and this is associated with cancer, cardiovascular disease and decreased physical function.
It is important to feed the body in a way that optimises your own health, and the hard part is crafting the right diet for your body's and mind's needs. What works for one person, will not necessarily work for somebody else, this is down to genetics and unique body chemistry.
What can you do to help yourself eat well? Here are five top tips:
- Drink Water – Depending on your gender and the amount you exercise will depend on how much water your body needs, aim for about 2 litres per day and see how you feel, you may need less, or you may need more!
- Eat at 5 Portions of Fruit and Vegetables a Day – These are good source of fibre, vitamins and minerals
- Eat 'Real' Foods – Actual food that came from the ground or had a mother ('Macaroni and cheese did not have a mother', Dr Suzanne Judd, University of Alabama)
- Eat Breakfast – When you break the overnight fast with a healthy breakfast, it's easier to resist unhealthy choices during the day
- Practice Mindful Eating – Allowing you to slow down and savour your food, which can help with overeating
Mental Health
 Mental Health is equally important as your physically health. In fact, the two are powerfully linked together, with one effecting the other and vice versa.
Mental Health is equally important as your physically health. In fact, the two are powerfully linked together, with one effecting the other and vice versa.
Mental Health has been defined by the World Health Organisation (2014) as:
'a state of well-being in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community'.
It has been estimated that 1 in 4 people will be affected by a mental or neurological disorder within their lifetime. The likelihood is that this figure is higher, especially in our current world of living with COVID. This is due to the uncertain nature of the world we find ourselves in.
Mental health should be seen as a continual process, same as physical health.
A mental illness is a condition that affects a person's thinking, emotions and behaviour, and disrupts the person's ability to work or carry out other daily activities and engage in satisfying personal relationships. Some people have only one episode of mental illness in their lifetime, while others have multiple episodes and periods of wellness in between.
Mental Health Symptoms
Signs and symptoms of mental health issues can vary, depending on the disorder, circumstances and other factors – affecting emotions, thoughts and behaviours. Examples of signs and symptoms include:
- Feeling sad or down
- Confused thinking or reduced ability to concentrate
- Excessive fears or worries, or extreme feelings of guilt
- Extreme mood changes of highs and lows
- Withdrawal from friends and activities
- Significant tiredness, low energy or problems sleeping
- Inability to cope with daily problems or stress
- Problems with alcohol or drug use
- Major changes in eating habits
- Excessive anger, hostility or violence
- Suicidal thinking
In addition, some symptoms of mental health issues can appear as physical problems, such as stomach pain, back pain, headaches, or other unexplained aches and pains.
Most mental health issues do not improve on their own, similar to physical health issues, and if left untreated, a mental health issue may get worse over time and cause serious problems.
Mental Health Causes
 In general, mental health issues are thought to be caused by a variety of genetic and environmental factors:
In general, mental health issues are thought to be caused by a variety of genetic and environmental factors:
- Genetics – Certain genes may increase the risk of developing a mental health condition, and a life event may trigger it. It is common that if there is a blood relative who has a mental health condition then this can be passed on as an inherited trait.
- Environmental Exposures During Development – Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs within the womb can sometimes be linked to mental health conditions.
- Brain Chemistry – Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When the neural networks involving these chemicals are impaired, the function of nerve receptors and nerve system changes, lead to depression and other emotional disorders.
Mental Health Top Tips for Prevention
 There is no prescribed method for preventing a mental health issue. However, there are things you can do to control stress, increase your resilience and boost low self-esteem, which may help keep the symptoms under control:
There is no prescribed method for preventing a mental health issue. However, there are things you can do to control stress, increase your resilience and boost low self-esteem, which may help keep the symptoms under control:
- Pay Attention to Warning Signs – work with your doctor, counsellor or even friends and family, to learn what triggers your symptoms. Make a plan, so you know what to do if symptoms return. Learn to reach out if you notice any changes in symptoms or how you feel.
- Get Help When You Need It – Mental health conditions can be harder to treat if you wait until symptoms get bad. Long-term maintenance treatment also may help prevent a relapse of symptoms.
- Take Good Care of Yourself – Sufficient sleep, healthy eating and regular physical activities are important, not only to your physical health but also your mental health.
General Tips for the Prevention of Poor Mental Health
- Keep your normal routine, getting up and going to bed at the same time
- For every hour you are sat down working, don't forget to get up and get moving for 10 mins – stretching, walking around your home, etc
- Take your lunch break away from the area you work in
- Regularly check in with your team and other colleagues. Just send a message, saying 'how are you doing?' really helps
- Sleep – If you are struggling, there are things you can do
- Reduce the light in your home as the evening goes on, this will naturally stimulate melatonin in your brain
- Have a bath, this will help reduce your core temperature, which helps the brain sleep, by moving the blood to your extremities and reducing brain temp
- Sleep in a dark, cool room, again this helps the brain switch off
- Avoid reading using an iPad (or similar device), the light from these devices stimulates the waking brain
- Avoid caffeinated and alcoholic beverages at least 2 hours before bedtime, both are stimulants, and although you may think alcohol helps you sleep, it doesn't help the appropriate sleep function in the brain
SOAP
SOAP© | Surface, Object, Area, People
Surfaces and COVID-19

Contact from infectious respiratory droplets through coughing and sneezing is one method of transmission, the spread via surfaces (technically known as fomite), where if somebody for example sneezed on a stainless steel surface, the virus can survive up to 72 hours (but not reproduce) before being picked up by somebody else who touches their nose, mouth and eyes and gets infected.
You cannot see the virus with your eye, SARS-CoV-2 is approx. 100nm, therefore when you are in not in your home and you are in places where lots of people are or have been, you should think before you touch any surface or object.
Carrying out a SOAP assessment
SOAP assessments are designed so that an individual or a group of personnel can risk assess in a COVID Environment with a systematic approach to risks.
It can be used in any environment and gives a tangible risk mitigation system.
Broken down into a mnemonic SOAP, the model actively educates your workforce in COVID risk reduction measures.
Surface – Object – Area – People
Surface
 Assessing surfaces that a person may encounter, for example, door handles, lift buttons, ATM machine buttons, packaging, workstation surfaces and any surface that may be contaminated with the COVID-19 virus.
Assessing surfaces that a person may encounter, for example, door handles, lift buttons, ATM machine buttons, packaging, workstation surfaces and any surface that may be contaminated with the COVID-19 virus.
The virus has been shown to stay on the following surfaces for the time indicated (Van Doremalen, N., et al., 2020. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Eng J Med, 382(16), pp.1564-1567; Chin, A., et al. 2020. Stability of SARS-CoV-2 in different environmental conditions. medRxiv.)
- Air = 3 hours
- Copper = 4 hours
- Cardboard = 24 hours
- Stainless Steel = 48 hours
- Plastic & Cotton = 72 hours
- Surgical Mask & Latex Gloves = 96 hours
- Glass & Ceramics & Wood & Paper = 120 hours
Objects
In line with surfaces, this part of the assessment is designed for people to be aware of objects that they may come into contact with that may be contaminated with the COVID-19 virus, for example, cups & glasses, magazines & leaflets, shopping trolleys & baskets, and anything that can be touched by people outside of your household.
Area
Area is a critical part of the assessment process and should be assessed alongside the S & O sections above. Looking at and within the area you find yourself, for example, lift, shops, pubs, you should look for active COVID measures either by physical markings or placement of furniture and systems that control movements.
The more active measures in place, for example, spatial distance markers, one-way systems, and advisory signs, the lower the risk the area could be COVID infected. The fewer control measures, the higher the risk.
For example, seating plans on a bus – bus companies have implemented seat closure signage and standing signage to create effective social distancing. The same has been seen in shopping locations with one-way movement signage and seating plans as well as decontamination points.
Entry into stores uses alcohol-based gels to use prior to entry. Some locations use entry systems manned by personnel as well as track and trace systems. All of these measures can be assessed as an area assessment using the SOAP model.
People assessments
When entering an area, you should assess the people to establish if they are a risk or they are aware to mitigate the risks? Assessing people whether they are wearing RPE, is a good quick assessment, this should be followed up with, are they wearing their RPE correctly? This will indicate an individual's approach to COVID, it could also indicate that they may be in a vulnerable group or are they protective of themselves and others.
What is their spatial distance like in areas? Are they spatially aware in an area? Do they observe the AREA markings or are they non-compliant?
All of these observed assessments build your personal COVID-aware risk assessment.
Summary of the SOAP Model
When operating in a COVID environment, you can use the SOAP model to assess risk as a unified method. Rather than assess each location with a multiple of risks, the SOAP model has been designed for people to have a high or low-risk level initial attitude.
When moving into new environment, for example, from commute (public transport) to office locations, the SOAP model can be used to assess initially as a high-risk location with areas potentially contaminated with the COVID virus.
The SOAP model unifies an approach and provides an assessment based on observations and knowledge.
Appendix
Appendix
The appendix contains some simple visual guides and information to help you understand more about COVID-19 and mitigate its risks.
COVID Symptoms Chart
Physical Distance Guide
How to Wash your hands
Track and Trace DIY
Organisations should consider methods that they can implement for their own businesses to track and trace employees with COVID symptoms.
Health Declaration/Questionnaire/Reporting mechanism
- For your own staff
-
- Cardinus can provide a symptom comparison chart
- Ensure all staff know what to do, if they develop symptoms
- Cardinus can provide a Track and Trace guide
- Ask staff to complete a health declaration every working day
- Alternatively, a method that all staff are aware of, if they develop symptoms whether they are in work or not, that they can report back to the organisation
- For the person who has visitors
- Wherever possible, try and keep a list of people that your visitor has come into contact with
- Wherever possible, try and keep your visitor from interacting with other staff
-
- For visitors
- All visitors to complete a health declaration
- Wherever possible, this should be sent in advance, and completed no more than 24 hours prior to visiting your location
- Request that visitors, if they develop COVID-19 like symptoms following 48 hours of visiting your location, that they inform the person they were visiting
- To send any risk assessment and method statement to the visitor, if you have protocols in place, such as wearing of PPE whilst on-site
- All visitors to complete a health declaration
What happens if somebody in your workplace shows symptoms of COVID-19?
If someone in your workforce develops symptoms of COVID-19 there is a method that can be implemented to identify who they have been in contact with, thereby allowing you to notify staff who may have been in contact with them to stay home.
Use the 2 – 15 – 48 Rule
The 2 – 15 – 48 rule is a simple method of finding out who the person has been in contact with.
- 48 = 48 hours – who has the person been in contact with in the past 48 hours before showing symptoms of COVID-19?
- 15 = 15 mins – in that 48-hour period, who has the person been in contact with for 15 mins (or more)?
- 2 = 2m – during that 15 min (or more) period, who has the person been in close contact with, within a 2m distance?
- Gathering this information will help you inform other people working in your environment that they may be at risk of developing COVID-19 and they should self-isolate.
Useful Links
Useful Links
Below is a collection of useful links to help you quickly access information about COVID from Government sources , charities and other resources.
COVID General
England – https://www.gov.uk/coronavirus
N Ireland – https://www.nidirect.gov.uk/campaigns/coronavirus-covid-19
Scotland – https://www.gov.scot/coronavirus-covid-19/
Wales – https://gov.wales/coronavirus
Travel
England – https://www.gov.uk/guidance/coronavirus-covid-19-travel-corridors
N Ireland – https://www.nidirect.gov.uk/articles/coronavirus-covid-19-travel-advice
Scotland – https://www.gov.scot/publications/coronavirus-covid-19-public-health-checks-at-borders/
Wales – https://gov.wales/coronavirus-travel
NHS – Check your symptoms – https://111.nhs.uk/covid-19/
Pregnancy – Royal College of Obstetricians and Gynaecologists – https://www.rcog.org.uk/en/guidelines-research-services/coronavirus-covid-19-pregnancy-and-womens-health/
Asthma – https://www.asthma.org.uk/coronavirus/
Mental Health Support:
-
- Mental Health Foundation
- Champion Health
- NHS
- Mind
- Centre for Mental Health
- Mental Health at Work
Dementia – https://www.dementiauk.org/get-support/coronavirus-covid-19/
Older people – https://www.ageuk.org.uk/information-advice/coronavirus/